Histopathological Pattern of Central Nervous System Infection: Experience of 61 cases at Referral Neuroscience Hospital in Bangladesh
Huq N,1 Haque ME,2 Jahan N,3 Yusuf MA,4 Baqui MN,5 Rozhana S,6 Shirin S,7 Islam MN8
Abstract
Background: Central nervous system (CNS) infections presenting as space occupying lesions are not uncommon in a developing country like Bangladesh.
Objective: The purpose of the present study was to see the histomorphological pattern of CNS infections.
Methodology: This retrospective study was carried out in the Department of Neuropathology at National Institute of Neurosciences & Hospital (NINS&H), Dhaka, Bangladesh during the time period of June 2013 to March 2018 for a period of around five (05) years. All the patients biopsied in neurosurgical department and was reported as infectious lesions from the Department of Neuropathology of NINS&H were selected as study population.
Result: A total number of 2504 cases of surgical specimens were reported during the study period of which 61(2.4%) cases were infectious lesions. Among 61 infectious cases tubercular lesion, suppurative and fungal causes of infection were found in 33(54.1%) cases, 21(34.4%) cases and 7(11.5%) cases respectively. Majority of the study population was in less than 40 years of age group which was 48(80.0%) cases. Male was predominant than female which was 38(62.3%) cases and 23(37.7%) cases respectively.
Conclusion: In conclusion tubercular infection is the most common CNS infection followed by suppurative and fungal infection.
[Journal of Histopathology and Cytopathology, 2019 Jul; 3 (2):143-150]
Key words: CNS infection, Tuberculosis, Fungal infection
- *Dr. Naila Huq, Associate Professor, Department of Neuropathology, National Institute of Neurosciences & Hospital, Dhaka, Bangladesh. nailahuqpopy@gmail.com
- Mohammad Enamul Haque, Senior Consultant, Victoria Hospital, Narayanganj, Bangladesh. doctorenamk43@gmail.com
- Nasreen Jahan, Research assistant, National Institute of Neurosciences & Hospital, Dhaka, Bangladesh.dr.nasreen2014@gmail.com
- Md. Abdullah Yusuf, Assistant Professor, Department of Microbiology, National Institute of Neurosciences & Hospital, Dhaka, Bangladesh. ayusuf75@yahoo.com
- Nazmul Baqui, Senior Lecturer, Unit of Pathology, Faculty of Medicine, AIMST University, Kedah, Malaysia. doctornazmul@yahoo.com
- Sharmin Rozhana, Lecturer, Unit of Microbiology, Faculty of Medicine, AIMST University, Kedah, Malaysia. srozhana@gmail.com
- Sadia Shirin, Medical Officer, Department of Neuropathology, National Institute of Neurosciences & Hospital, Dhaka, Bangladesh. sadiashirin77@gmail.com
- Md. Nowfel Islam, Professor & Head, Department of Pathology, National Institute of Neurosciences & Hospital, Dhaka, Bangladesh. nowfel2008@gmail.com
*For correspondence
Introduction
Top of FormBottom of FormDiseases causing multiple ring enhancing lesions of the brain are infectious, neoplastic, inflammatory or vascular origin.1-3 Central nervous system (CNS) infections are important because of many emerging and reemerging pathogens. Now a day’s persons are at increased risk of CNS infection due to acquired immunodeficiency syndrome (AIDS). CNS becomes a watershed for Human Immunodeficiency Virus (HIV) infection.4 Infections are also common among the recipients of organ transplantation.2-5 Infections are caused by a wide variety of organisms including bacteria, fungi, parasite and virus. Environmental factors in tropical countries play a significant role in the pathogenesis of CNS fungal infections. Immunocompromised patients are commonly susceptible to fungal infection.5 But exposure to drug or contaminated devices can also cause CNS fungal infection in immunocompetent person. Even People of endemic region can get CNS infection following heavy exposure to fungi.4, 6
Radiology is not always helpful for the diagnosis of CNS infection. Some treatable infectious diseases can even mimic the MRI features of demyelinating disease like multiple sclerosis.3,7,5 Although neoplasms are the common considerations in the presence of enhancing lesions with perilesional edema and mass effect on neuroimaging; non-neoplastic conditions particularly, infectious lesions can have similar imaging characteristics.1
Histopathological diagnosis is essential in case of neoplasm for diagnosis, grading as well as treatment. But infectious lesions that could not be diagnosed by noninvasive procedure also need biopsy. Distinguishing non-neoplastic from neoplastic lesion is extremely important to relieve the patient from the potential side effect of chemotherapy and radiotherapy.3 On the other hand, though brain infections are rare but due to limited space and involvement of vital areas they are associated with high morbidity and mortality.2,8
As Bangladesh has conservative society; HIV infection is not so common. However, like other part of the world, Bangladesh deals with a considerable number of patients having organ transplantation. Moreover, it is one of the densely populated countries of the world. Communicable diseases impose heavy burden on health care system. Tuberculosis is an emerging global health problem. In a country with huge population burden, poor hygiene, malnutrition, less health awareness of people, tuberculosis as well as other infections with involvement of CNS is not rare. There are a very few study regarding the frequency or prevalence of CNS infection in Bangladesh. This study was focused on the frequency and distribution pattern of CNS infections in Bangladesh.
Methods
The present retrospective study was based on the data collected from the Department of Neuropathology NINS&H, Dhaka, Bangladesh during the time period of June 2013 to March 2018 for a period of around five (05) years. In this study the data of the patients who were underwent CNS surgery and histopathologically diagnosed as infectious lesions were collected. Cases of meningitis were not included in this study as diagnosis of meningitis based only on CSF examination. All extra-cranial skin, soft tissue and bony infectious lesions were excluded from this study. Specimens were stained by routine Hematoxyline & Eosin (H&E) stain. Furthermore, Zeihl-Neelsen stain was performed in all cases of tuberculosis. Periodic Acid Schiff (PAS) stain was done in all cases of fungal infection. Statistical analyses were performed by Statistical Package for Social Science (SPSS) software, versions 22.0 (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.). Continuous data that were normally distributed were summarized in terms of the mean, standard deviation and minimum, maximum. Categorical or discrete data were summarized in terms of frequency and percentages.
Result
A total number of 2504 cases of surgical CNS specimens were reported during the study period of which 61(2.4%) cases were infectious lesions. Only cases of infectious lesions were further analyzed. The age range of patients was 9 months to 85 years. The patients were stratified into 4 groups which were less than 20 years, 20 to 40 years, 40 to 60 years and more than 60 years. Most of the patients belong to 20 to 40 years age group which was 26(42.6%) cases followed by less than 20 years which was 23(37.7%) cases. CNS infection was very rare in more than 60 years of age; only two cases were found in this age group. However, male predominance with a male to female ratio of 1.7:1 was seen. Male was 38(62.3%) cases and female 23(37.7%) cases respectively (Table I).


In 61.0% cases of histologically diagnosed CNS infections radiological diagnosis were tumors. However in 39.0% cases radiological diagnosis was infection which correlates with the histological diagnosis. In 19 cases radiological diagnosis correlates with the histopathological diagnosis and all of them were tubercular lesion. Radiological diagnosis did not correlate with histopathological diagnosis in 32 cases. And radiology was not available in 10 cases.

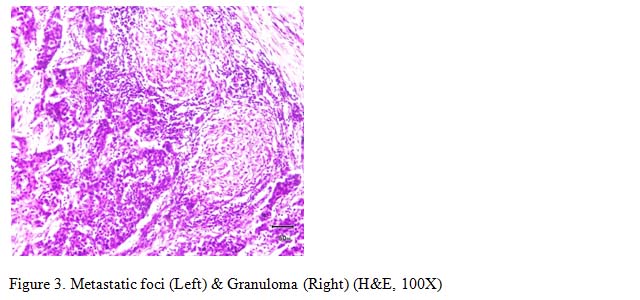
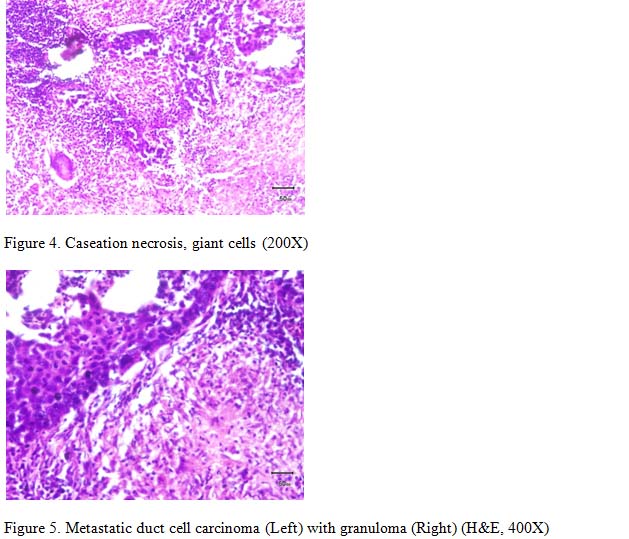
Of the total 61 cases 33(54.1%) cases were tubercular, 21(34.4%) cases were suppurative and 7(11.5%) cases were fungal infection. AFB stain done in 30 cases of tuberculosis and result was negative. All cases of fungal infection were further stained by PAS stain and found positive.
Discussion
CNS includes a wide variety of diseases ranging from suppurative, tubercular, fungal, parasitic and viral infection. For the diagnosis of these cases combined approach of clinical, radiological, CSF and histopathological examination are necessary. There is a scarcity of research works related to the pattern of CNS infections in Bangladesh. As National Institute of Neurosciences & Hospital (NINS&H) is a tertiary level referral hospital in Bangladesh, it deals with different neurological diseases having a well-developed neurosurgery department. Therefore, a great number of patients attend in this hospital.
CNS infection producing space occupying lesions are not uncommon in Bangladesh. About 2.4% of surgical specimens of this study belong to infectious lesions. The age range of the study population was 9 months to 85 years with highest percentage 42.6% cases between 2nd to 4th decades, followed by 37.7% cases in less than 20 years. CNS infection was very rare in more than 60 years of age; only two cases found in this group. The age distribution is consistent with most of the previous studies conducted in different parts of India.9,10,11 In our study 62.3% cases were male and the male to female ratio was 1.7:1. A male predominance seen in most of the reported studies indicating that male are more prone to these infections.9,10,11 This may be due to more exposure of the male of this age group to the environmental agents, vectors due to their outward activities.9 Some zoonotic infections like Neurobrucellosis occur due to occupational exposure.12 Moreover, in the developing countries male got priority over the female in getting treatment facilities.9 This observation matches with Bangladesh having the similar socioeconomic pattern.
We analyzed the anatomical location of the total 61 cases. It has been observed that most of the cases 49(80.0%) were cranial and 12(20.0%) cases were in spinal location. The percentage could be different if lesion like Pott’s disease would include in the study. Rosenblum5 has reported that 20.0% of brain abscess are not associated with predisposing bacterial infection; however, remaining results are from established pyogenic infection in extraneural site. Contiguous spread of infection can result from sinusitis, otitis, dental sepsis and pyogenic infection of face and scalp which causes intracerebral abscess or subdural empyema.5 Contamination of the CNS can occur in three routes. Arterial route is the main route of contamination and the disposition of intracerebral arterial division causes development of diseases in this way at the junction of white matter and gray matter or in the territory of perforating artery. Therefore, frontal or temporal region lesion is most common. Spinal anomalies predispose to intramedullary abscess but such infections are extremely rare5. Herpes simplex, Rabies, Varicella Zoster or a few viruses disseminated through neural route. Direct contamination can result from cranial or vertebral wound or following intracranial surgery. All these explanations suggest that cranial location is more common site of CNS infection particularly in case of acute bacterial infection which is similar to our study.5,8 Another study has been mentioned that infectious lesions in the brain stem are very rare.13
Among 61 cases radiology is not available in 10 cases which are histologically diagnosed as CNS infection. In the remaining, radiological diagnosis correlates with the histopathological diagnosis in 39.0% cases. However, in 61.0% cases radiological diagnosis are tumors. From biostatistical point of view it is not the indicator of sensitivity of radiology. As cases of CNS tumors were not included in the study, it would be a biased statement.
In radiology, neoplasm is the common consideration in enhancing lesions with perilesional edema and mass effect. But infectious lesion, occasionally demyelinating disease can share the similar imaging characteristic1,5. There are some limitations of early imaging and overlapping imaging appearance of many of the infections. Pyogenic abscess often show amino acid at spectroscopy. Neurotuberculosis, neurosyphilis shows nodular meningeal enhancement with or without vasculitis which can also be seen in fungal infection. Some diseases like, neuro-cysticercosis, echinococcosis may have highly characteristic imaging pattern. But many other infections share common imaging findings. So, a high degree of suspicion is required to assume the diagnosis of CNS infection in radiology.1,14
Of the total 61 cases 54.1% cases are tubercular; 34.4% cases are suppurative and 11.5% fungal. As primary tuberculosis has high prevalence in Bangladesh, CNS tuberculosis might be the commonest presentation in this study. Garg RK3 et al also mentioned intracranial tuberculoma as frequently encountered brain lesion in tropical country. Bacteria are responsible for majority of suppurative infections of CNS and its covering.5 According to working criteria, cases of meningitis are not included in this study. Pyogenic abscess is the second common presentation (34.4% ). Our study is limited by non-availability of relevant microbiological analysis. So type of organism producing pyogenic abscess could not be determined from this study.
We found 7 cases of fungal infection. One of them was suffering from rheumatoid arthritis and receiving treatment with methotrexate. And another was a baby of 9 monthsage. Rest of the patients has no known history of immunodeficiency. Incase of fungal infection we found highest incidence of aspergillosis(4) followed by zygomycosis(2). Only one case of phaeohyphomycosis was found. A hospital based study of India also shows increased incidence of hyphal form like aspergillosis and Zygomycosis in non immunocompromised host.15The cryptococcus usually causes meningitis and rarely presentas cryptococcoma.16,17 Therefore, the cryptococcus is not found in this study.
CNS parasitoses include a great variety of protozoa and helminth.5,17 We did not find any case of neurocysticercosis, toxoplasmosis, echinococcosis, malaria, schistosomiasis and also rare amoebic infection of CNS. A study in India by Bhalla et al9 showed that these infections produce intracranial mass lesion in HIV positive patients. An HIV infected patient having CD4 cell count less than 200 cells/µL is at high risk for opportunistic brain infection. HIV infection is not so common in Bangladesh in comparison with other South Asian country like India or Thailand. As patients of HIV get treatment only in Infectious Disease Hospital (IDH) of Bangladesh, the data of those patients could not be included in this study. These infections may be less frequent in our environment or poor access of our people to the tertiary level hospital like NINS&H may result such outcome. As most of the affected people belong to lower socioeconomic condition the people may die before reaching the health care system. Another study in India showed that some of these infections of nervous system diagnosed mostly in autopsy specimen.5,18 A study in Hill tracts of Bangladesh; endemic for malaria showed significant cases of cerebral malaria in autopsy specimens.19 As facilities of autopsy are not available in our institute the study might be missing these infections.






Conclusion
Tubercular infection is the most common CNS infection followed by suppurative and fungal infection in biopsied specimen. Less than 40 years age group is the most vulnerable age group. High clinical suspicion, awareness of imaging pattern and microbiological approach can minimize the need for brain biopsy. Further large scale multi-institutional study including autopsy should be carried out.
References
- Santosh V, Mahadevan A, Chickabasaviah YT, Bharath RD, Krishna SS. Infectious lesions mimicking central nervous system neoplasm. Semin diagn pathol, 2010;27(2):122-35
- Sundaram C, Shankar SK, Thong WK, and Villamizar CAP. Pathology and diagnosis of Central nervous system infections. Pathology Research International, 2011, Article ID878263:1-4
- Garg R K, Singha M K, Multiple ring-enhancing lesion of the brain. Journal of Postgraduate Medicine 2010;56(4):307-316
- Wig N, Wali JP. Central nervous system and HIV/AIDS. Journal of Indian Academy of Clinical Medicine Vol. 2008;5(2):164-168
- Rosenblum MK. Central nervous system in Rosai and Ackermans Surgical Pathology.10th vol.2,2327-2338
- Rodriguez T. Fungal infection of the CNS: Diagnostic and Treatment Approaches. Neurology adviser, 2018 May, 1-8; Website: https://www.neurologyadvisor.com/topics/general-neurology/fungal-infections-of-the-cns-diagnostic-and-treatment-approaches/
- Rocha AJD, Littig IA, Nunes RH, Tilbery CP. Central nervous system infectious diseases mimicking multiple sclerosis: recognizing distinguishable features using MRI. Arq Neuropsiquiatr 2013;71(9-B):738-746
- Sarrazin J-L, Bonneville F, Blondel GM. Brain infections in Diagnostic and Interventional Imaging 2012;93:473-490
- Bhalla A, Kharbanda PS. Tropical CNS infections: one must not forget. Update on Tropical Fever 2011;75-86
- Joshi R, Clinical presentation, etiology and survival in adult acute encephalitis syndrome in rural Central India in Clin Neurol Neurosurg.2013;115(9):1753-1761
- Modi A, Atam V, Jain N, Guth M, Verma R. The etiological diagnosis and outcome in patients of acute febrile encephalopathy: a prospective observational study at tertiary care center. Neurol India 2012;60(2):168-173.
- Algahtani H, Shirah B, Abdulghani D, Farhan R, and Algahtani R,Occapational Neurobrucellosis Mimicking a Brain Tumor: A Case Report and Review of the Literature in Case Report in infectious Diseases ;Volume 2017, Article ID 1434051:1-5
- Hall WA, Infectious lesions of the brain stem in Neurosurg clin N Am. 1993;4(3): 543-51
- Robert Y. Shih LTC, Kelly K. Koellar, MD Bacterial, Fungal and Parasitic Infections of the Central Nervous System: Radiologic-Pathologic correlation and Historical perspectives. Radiographics 2015;35(4)4:1141-1169
- Shankar SK, Mahadevan A, Sundaram C, Sarkar C, Chako G, Lanjewar D N, Santosh V, Yasha TC, Radhakrishnan V. Pathobiology of fungal infections of the central nervous system with special reference to the Indian scenario. Neurology India 2007;55(3):198-215
- Gupta K, Radotra B. Non-neoplastic Lesions Mimicking CNS Tumors. Essentials of Diagnostic Surgical Neuropathology: 230-239
- Matthew P. Frosch, Douglas C. Anthony, Girolami UD, The central nervous system in Robbins and Cotran, Pathologic basis of disease, eighth ed. 1299-1309
- Shankar SK, Mahadevan A, Parmar S, Histological Atlas of Common Infections of the Nervous System With Teaching Slides:1-64
- Islam SMJ, Uddin MJ, Haque WS, autopsy findings in cerebral malaria, Journal of Armed Forces Medical College Bangladesh, December 2006; vol 2(2).